Treating and Preventing Opioid Overdose
The Bottom Line
When it comes to the opioid epidemic, we can all have a positive impact regardless of our social, economic, or professional status. It is important to practice safe medication use, storage, and disposal to prevent poisoning. By learning how to use the opioid reversal agent naloxone, you could save a life. Learn more by listening to our podcast, Poison!.

The Full Story
Although the opioid epidemic is occurring on a large scale it can still be affected by individual actions. Recognizing, treating, and preventing opioid overdose is discussed in depth in our podcast episode, "Be Prepared, Save a Life."
First, you should know how to recognize an opioid overdose. Signs of an opioid overdose can include the following:
- Not waking up or not responding to voice or touch
- Skin is pale, gray, and clammy
- Lips and fingernails turning blue or purple
- Breathing is very slow, irregular, or has stopped
- Slow heartbeat or low blood pressure
- Pinpoint pupils (the center circle of the eye is very small)
It is important to know that not all of these signs will necessarily be present.
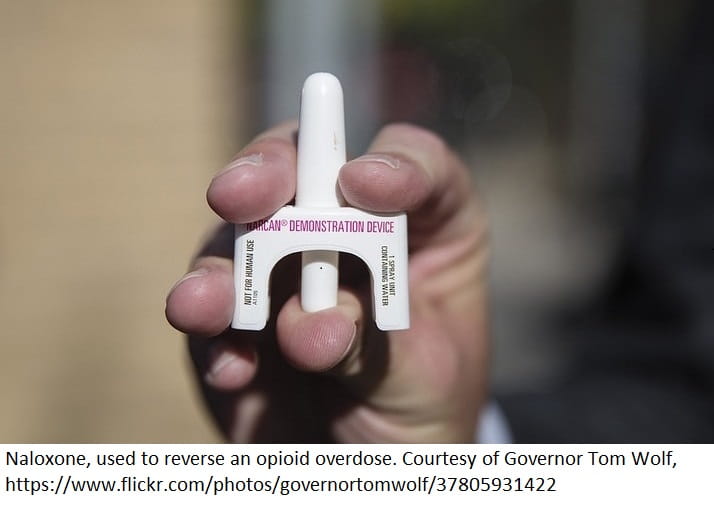
Second, always have the reversal agent available and know how to use it. The reversal agent for opioid overdose is naloxone. It can be given as a nasal spray, an injection, or as an intravenous infusion. The nasal spray products and some auto-injectors are intended for the public and come with instructions for use; it is best to familiarize yourself with the instructions before an overdose occurs. This medication is safe to use in all people experiencing a life-threatening overdose, even during pregnancy. Naloxone temporarily prevents opioids from attaching to opioid receptors in the brain. Because its action is temporary, multiple doses might be necessary when a long-acting opioid has been taken.
As of June 2018, all states except Nebraska allow patients to get naloxone from any pharmacy without a prescription. However, because of the social stigma surrounding drug use and abuse, naloxone can be difficult to acquire despite the laws put in place to increase access to this vital rescue agent.
If you think someone is experiencing an opioid overdose, follow these steps:
- Call 911 first!
- Shake the person's shoulders and in a loud, clear voice call their name and ask if they are OK.
- If they do not respond, perform a sternal rub by making a fist and firmly rubbing the center of their breastbone with your knuckles. This hurts and tests for unconsciousness in patients who do not respond to sound.
- Give naloxone according to the package instructions.
Any patient who uses an opioid, whether it is legal or illegal use, should have access to and know how to use naloxone. This agent is not reserved only for patients with substance abuse disorder. Unintentional overdose can happen at any time, to any person, and in any place. Do not let a perceived social stigma put you or your family members at risk for overdose and death.
In some cases, bystanders witnessing an opioid overdose have not called for help because they were worried about being arrested for drug-related crimes. To encourage people to seek out medical help in overdose situations, 40 states and the District of Columbia have adopted "Good Samaritan" or "911 drug immunity" laws that give certain legal protections to people who call for help in the event of an overdose. The scope of what is covered by these laws can vary by state, and you should familiarize yourself with your state's laws.
Although naloxone is an effective reversal agent, when it comes to opioids, prevention really is the best medicine. Rapid and appropriate disposal of narcotic medications can prevent unintentional exposure or intentional misuse. Visit the FDA Safe Disposal of Medicines website to review their recommendations for medication disposal. The US Environmental Protection Agency (EPA) warns against flushing medications down the toilet or drain unless the label or patient information for the medication instructs you to do so.
The US Drug Enforcement Administration (DEA) periodically holds National Prescription Drug Take-Back events with collection sites set up nationwide to accept and dispose of unwanted or unused medications. Local law enforcement agencies sometimes host similar take-back events and local waste management companies might have disposal guidelines or recommendations for your area.
Another option is to use DEA authorized collectors that will facilitate disposal of these medications. Visit the DEA website to locate your local DEA-authorized collectors.
If you are unable to use a DEA-authorized collector and if your waste management company allows, you can follow these steps to safely dispose of unwanted medicines in your household trash.
- Mix medicines (do not crush) with an unpleasant substance like dirt, kitty litter, or used coffee grounds.
- Place the mixture in a container such as a sealed plastic bag or coffee can and throw it into your household trash.
- Scratch out all personal information on the prescription label of your empty medicine packaging to make it unreadable, then dispose of the container.
When opioids have been abused by injection, another hazard emerges: needles that are used multiple times or by multiple people can easily spread illnesses like HIV/AIDS and hepatitis. One way to deal with the needle problem is through Syringe Services Programs (SSPs). These programs offer access to sterile needles, safe disposal of used needles, infectious disease testing, education regarding drug abuse, referrals to medical, mental, and social services, and much more. In addition to reducing the risk of injection-related illness among opioid users, these programs reduce the risk of illness following unintentional needlestick injuries in first responders and children. SSPs do not increase drug use or crime in the areas where they are located. People who use SSP resources are more likely to seek help for drug abuse treatment and limit use or stop injecting entirely.
Lindsy Liu, PharmD
Certified Specialist in Poison Information
Diana N. Pei, PharmD
Certified Specialist in Poison Information
Pela Soto, PharmD, BSHS, BS
Certified Specialist in Poison Information
Poisoned?
Call 1-800-222-1222 or
Prevention Tips
- Learn to recognize and respond to the signs of opioid overdose.
- Learn how to use the opioid reversal drug naloxone.
- Check FDA and DEA instructions before disposing of any unused medication.
- Support safe needle disposal sites in your community.
- Learn more about the opioid epidemic on our podcast.
This Really Happened
A 21-year-old man was found unconscious by his father after overdosing on heroin. Paramedics arrived and gave him naloxone. On the way to the ER, he stopped breathing and stopped responding to the naloxone. Once in the ER, the patient was again given naloxone. He became slightly more responsive and his breathing improved. During the course of his care it was discovered that he had developed a lung infection resulting from his coma, so he was treated with antibiotics. The day his father found him unconscious was the second time he had used heroin. He reported that he had overdosed each time he used the drug.
For More Information
References
DEA National Rx Take Back Day. Springfield VA: US Drug Enforcement Agency [accessed 20 May 2018].
Recognizing an opioid overdose. Radnor PA: ADAPT Pharma; 2017 [accessed 2 Jun 2018].
Poisoned?
Call 1-800-222-1222 or
Prevention Tips
- Learn to recognize and respond to the signs of opioid overdose.
- Learn how to use the opioid reversal drug naloxone.
- Check FDA and DEA instructions before disposing of any unused medication.
- Support safe needle disposal sites in your community.
- Learn more about the opioid epidemic on our podcast.
This Really Happened
A 21-year-old man was found unconscious by his father after overdosing on heroin. Paramedics arrived and gave him naloxone. On the way to the ER, he stopped breathing and stopped responding to the naloxone. Once in the ER, the patient was again given naloxone. He became slightly more responsive and his breathing improved. During the course of his care it was discovered that he had developed a lung infection resulting from his coma, so he was treated with antibiotics. The day his father found him unconscious was the second time he had used heroin. He reported that he had overdosed each time he used the drug.
